Osteoarthritis
Introduction
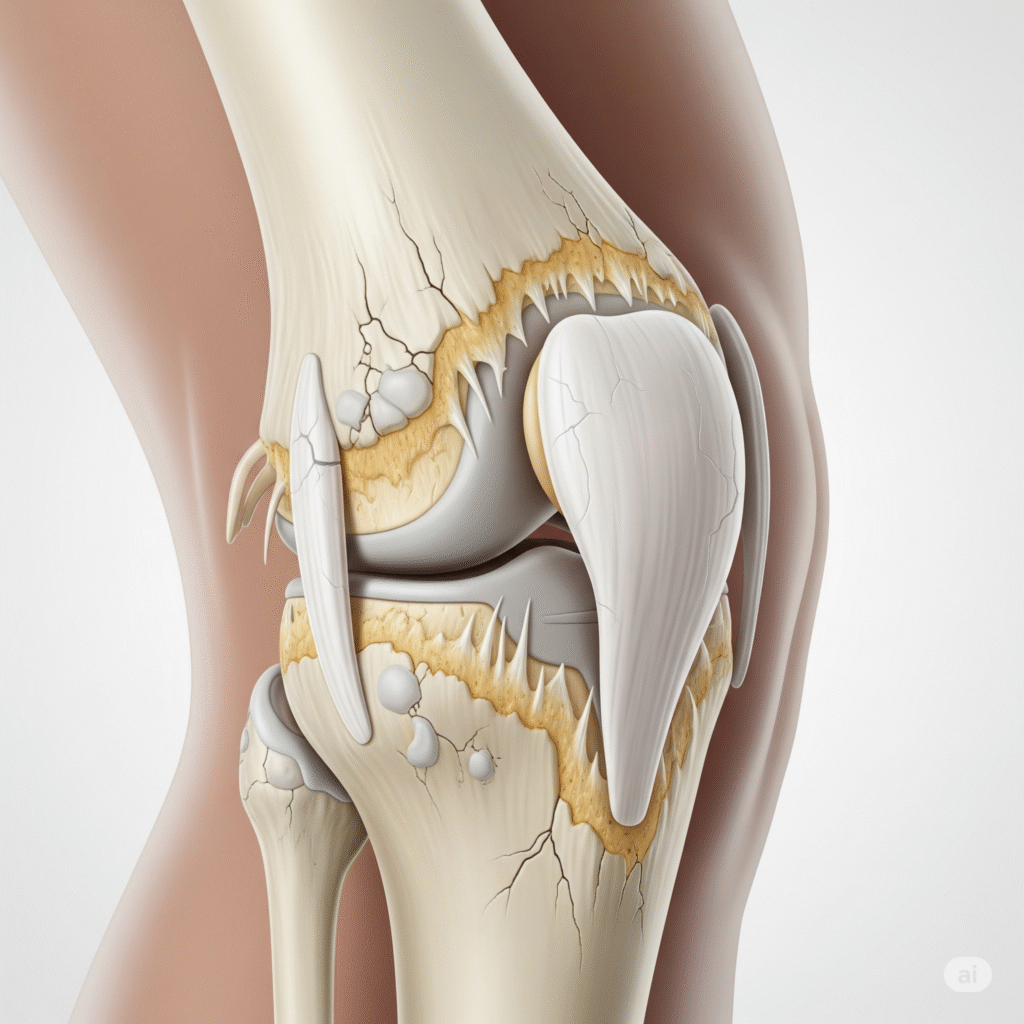
Osteoarthritis is the most common type of arthritis, caused by gradual wear and tears of joint cartilage. It leads to pain, hardness, swelling and low mobility, most often affects the knees, hips, hands and spine. The condition usually develops with age, but can also be caused by joint injury, obesity or excess use. Although it is a chronic disease, proper treatment and lifestyle changes can help relieve symptoms and improve joint function.
Types of osteoarthritis
Primary osteoarthritis
Any specific underlying underlying disease occurs, mainly due to aging of joint cartilage and natural degeneration.
Secondary osteoarthritis
Another condition develops as a result of diseases such as joint injury, obesity, or diabetes.
Tighten
A more severe and inflammatory form affects the small joints of most hands, causing pain and deformity.
Metabolic osteoarthritis
The previous joints rise after injury or fracture, causing early cartilage breakdown and long -term pain.
Causes of osteoarthritis
- Increasing age is the most common cause, because cartilage naturally wears over time.
- The risk of early cartilage damage increases in previous joint injuries or fractures.
- Obesity adds excess stress on weight-bearing joints such as knees and hips.
- Repeatedly over -use of joints with work, sports, or heavy physical activity intensifies the breakdown of cartilage.
- Genetic factor or family history may inspire individuals for early osteoarthritis.
- Weak muscles around the joints provide less support and increase joint stress.
- Poor posture or abnormal joint alignment creates uneven pressure, damaging cartilage.
- Metabolic disorders such as diabetes can contribute to joint degeneration.
- Inflammatory joint diseases, although separate, can increase the risk of secondary osteoarthritis.
- Lack of physical activity weakens muscles and reduces joint flexibility, deteriorating cartilage.
Clinical features of osteoarthritis:
Joint Pain
The most common feature, worsening with pain activity and improves with rest, especially in joints with knees and hips.
Joint rigidity
Hardness occurs mainly after morning or period of inaction, usually lasting for less than 30 minutes.
Swelling and tenderness
Cartilage wear and joint inflammation may cause light swelling to the affected joints, with tenderness.
Reduced Range of Motion
The movement is limited, making daily activities to walk, climb stairs, or it is difficult to catch objects.
Crepitus (Grating Sensation)
A cracking or hasty sound can be felt or heard during joint movement, which is caused by rough cartilage surfaces.
Symptoms associated with osteoarthritis:
- The joint pain deteriorates with activity and decreases slightly after proper comfort.
- The hardness of the morning makes the movement difficult, usually for less than thirty minutes.
- Inflammation causes discomfort, puffiness and heaviness around the joints affected by inflammation.
- Low speed limits flexibility, interfere with daily activities such as bending.
- Rough bones rub together during joint movement.
- Tenderness appears when the joints have mild pressure or pain on the touch.
- Bone spars cause stiffness, visible growth, and sometimes nerve compression cause pain.
- Muscle weakness reduces joint stability, increases injuries and risks of fall.
Investigations in osteoarthritis:
- A detailed clinical evaluation is the first step, where the doctor assesses the pain, hardness, swelling, tenderness, joint deformity and range of motion. It helps to separate osteoarthritis from other arthritic conditions and guides further investigation for diagnosis and treatment plan.
X-rays are the most common clinical tools, which reflect joint location narrowness, osteophytes (bone spurs), subcondral sclerosis and deformity. These findings confirm the progression and severity of osteoarthritis, helping doctors evaluate structural damage and planning appropriate treatment such as physiotherapy, drug or surgery.
MRI provides wide images of soft tissues, cartilage, ligaments and bone marrow. It helps in detecting cartilage losses and subtle changes that do not appear on X-rays. MRI is particularly useful when symptoms are severe but X-rays appear relatively normal.
Musculoskeletal ultrasound is useful in joint fusion, mucus thickening, cartilage changes and small osteophytes detecting. It is a safe, inexpensive and non-invasive tool that helps guide injection and monitoring disease activity to patients with osteoarthritis during follow-up treatment.
CT scan provides cross-sectional images of joints, showing detailed bony changes and alignment issues. It is particularly helpful in evaluating complex joints such as spine or hip where plain X-ray treatment can not provide adequate clinical information for the treatment plan.
Although there is no specific blood test for chronic osteoarthritis, routine testing helps to control other forms of arthritis such as rheumatism or gout. Tests such as ESR, CRP and rheumatoid factors are used to exclude inflammatory conditions.
The synovial fluid is aspirational from the affected joint and is examined for crystal, infection or inflammation. In osteoarthritis, the fluid is usually clear and non-inflammatory, helping to separate it from other conditions such as gout or septic arthritis.
Doctors can perform functional assessments such as gate analysis, running speed, seet-to-stand test and grip strength evaluation. These tests measure physiological boundaries and help determine how much osteoarthritis affects daily life, mobility and quality of the patient’s movement.
Arthroscopy is a minimum invasive process where a small camera is inserted inside the joint. This allows the direct view of cartilage damage, osteophytes and verbal changes. Although there is less common for diagnosis, it provides valuable information and sometimes medical benefits.
A bone scan involves injecting a small radioactive substance to detect bone growth activity. This stress is not clearly visible on the X-ray to fracture, bone remodeling, or early osteoarthritis changes, especially in patients in unexplained broad joints.
