Acute pancreatitis
Introduction
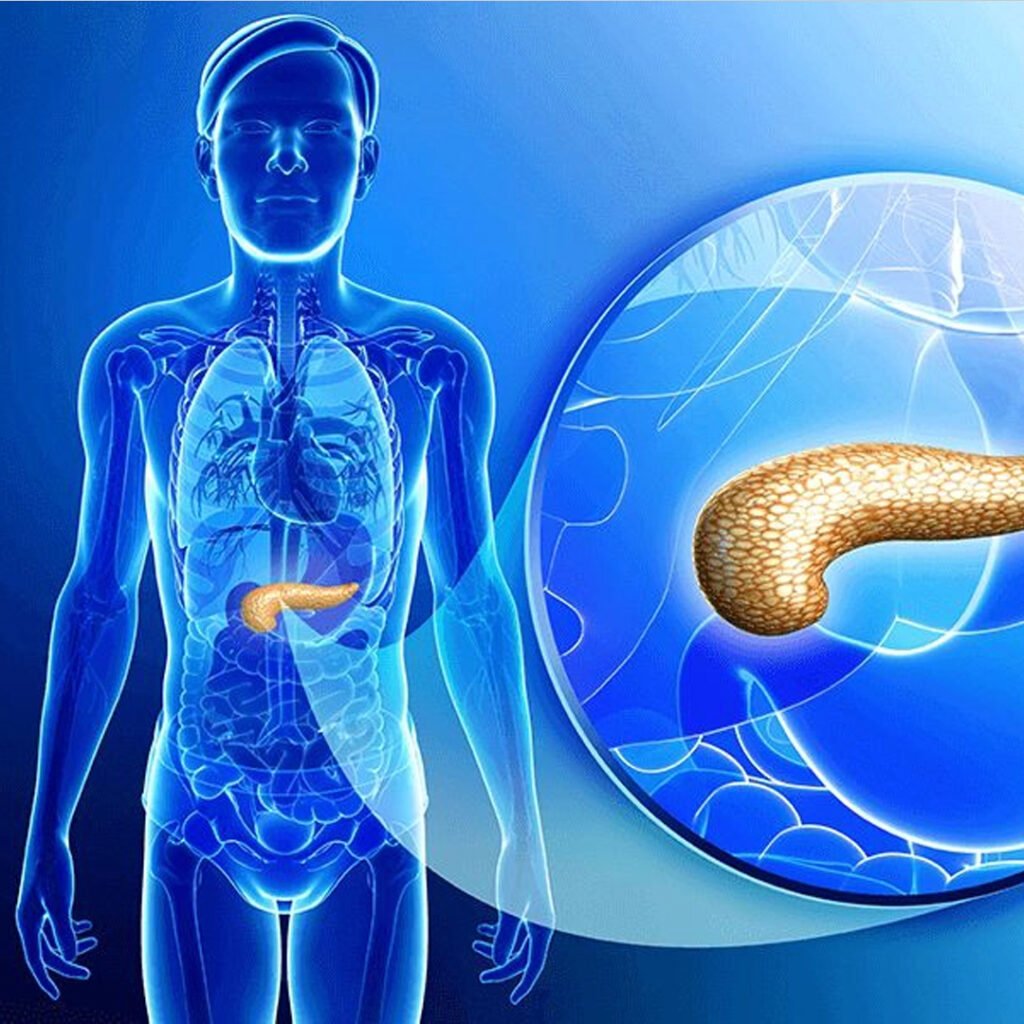
Acute pancreatitis is a sudden inflammation of the pancreas, an important organ responsible for the production of digestive enzymes and regulating blood sugar levels. This condition occurs when the digestive enzymes become active inside the pancreas instead of the small intestine, causing irritation and tissue damage. This can range from mild discomfort to serious, life-threatening disease. Common causes include bile stones, excessive alcohol consumption, certain medications, infections and stomach injuries. Initial diagnosis and treatment are necessary to prevent complications such as organ failure, infection and chronic pancreatitis.
Types of Acute pancreatitis
Mild acute pancreatitis (MAP)
Light acute pancreatitis causes limited pancreatic inflammation without organ failure and usually resolves quickly with conservative treatment and accessory medical care.
Mild severe pancreatic (msap)
Minor severe acute pancreatitis involves transient organ dysfunction or local complications, usually improved within a week with timely supporting management.
Severe acute pancreatitis (SAP)
Severe acute pancreatitis causes widespread pancreatic necrosis and frequent organ failure, requiring intensive medical care and sometimes surgical intervention for recovery.
Necrotizing acute pancreatitis (NAP)
Necrotizing acute pancreatitis occurs when pancreatic tissue dies due to severe inflammation, often leading to infection and life-threatening complications.
Causes of Acute pancreatitis
- The biliary stones block the bile duct, prevent enzyme flows and cause pancreatic inflammation and pain.
- Excessive alcohol intake damages pancreatic cells, causing enzyme activation and acute inflammation.
- High triglyceride levels increase fatty acids, causing pancreatic injury and acute pancreatitis episode.
- Some drugs disturb the pancreas, resulting in enzyme leakage and sudden acute inflammation.
- Stomach trauma directly damages the pancreas, irritates the enzyme function and causes inflammation.
- The pancreatic duct blocks the inhibiting enzyme drainage, causing inflammation and acute pancreatitis.
- Viral infection damages pancreatic cells, triggers inflammation and causes acute pancreatitis.
- The biliary stones block the bile duct, prevent enzyme flows and cause pancreatic inflammation and pain.
- Excessive alcohol intake damages pancreatic cells, causing enzyme activation and acute inflammation.
- High triglyceride levels increase fatty acids, causing pancreatic injury and acute pancreatitis episode.
- Some drugs disturb the pancreas, resulting in enzyme leakage and sudden acute inflammation.
- Stomach trauma directly damages the pancreas, irritates the enzyme function and causes inflammation.
Clinical features of Acute pancreatitis
Serious stomach pain
Suddenly, acute upper abdominal pain reaches the back, deteriorating after food or alcohol.
Nausea and vomiting
Frequent nausea with frequent vomiting is usually seen in cases of acute pancreatitis.
Abdominal Tenderness
The upper abdomen gets tender to touch, often associated with muscle guarding and inflammation.
Fever and rapid pulse
Infections and inflammation rapidly raise body temperature with weak pulse.
Jaundice
The obstruction of the bile ducts caused by the yellow skin and the tears of the eyes due to bile stones.
Symptoms associated with Acute pancreatitis
Severe upper abdominal pain reaches the back, deteriorating after meals.
- There is continuous nausea and vomiting due to pancreatic inflammation and irritation.
- Stomach accumulation and inflammation develops inflammation and inflammation of the stomach.
- Fever and chills are caused by pancreatic infection or systemic inflammation.
- Loss of fluid causes rapid heartbeat and low blood pressure.
- Lung participation or fluid around the lungs causes shortness of breath.
- Jaundice develops when the bile ducts are blocked by stones or inflammation.
- Excessive weakness and fatigue results from dehydration and systemic inflammatory reaction.
Investigations in Acute pancreatitis
- Serum amylase is an enzyme produced by the pancreas to aid digestion. In acute pancreatitis, amylase levels rise within a few hours of symptom onset. Elevated amylase indicates pancreatic inflammation, helping in early diagnosis. However, it may normalize quickly, so timing and correlation with symptoms are important for accuracy.
Serum lipase is a pancreatic enzyme more specific than amylase. Levels rise within hours of pancreatic injury and remain elevated longer. Measuring lipase helps confirm acute pancreatitis and assess severity. Persistent elevation can indicate ongoing pancreatic damage or complications, making it a reliable marker for diagnosis and monitoring.
CBC evaluates white blood cells, hemoglobin, and platelets. Leukocytosis indicates inflammation or infection, while low hemoglobin suggests bleeding. Platelet counts can reflect systemic stress or sepsis. CBC provides information on the body’s inflammatory response and helps identify complications such as anemia, infection, or systemic involvement in acute pancreatitis patients.
LFTs measure bilirubin, ALT, AST, and alkaline phosphatase levels. Abnormalities may indicate gallstones, bile duct obstruction, or liver involvement. Elevated bilirubin suggests obstructive pancreatitis. Monitoring LFTs helps determine the cause of pancreatitis, guides management, and identifies concurrent liver complications that require timely intervention.
Electrolytes such as sodium, potassium, calcium and chloride are monitored during pancreatitis. Vomiting, loss of fluid, and inflammation can cause imbalance, causing heart, neuromuscular, or kidney complications. Curing these imbalances is necessary for the stability of the patient and prevent systemic effects associated with acute pancreatitis.
Pancreatic inflammation can deteriorate insulin secretion, resulting in hyperglycemia. It is important to monitor blood sugar levels to prevent metabolic complications and manage effectively acute pancreatitis. Constant high glucose can indicate endocrity of endocrine pancreatic and require temporary insulin therapy or careful monitoring during recovery.
Abdominal ultrasound is a non-invasive imaging technique used to evaluate the pancreas, detect gallstones and assess ductal obstruction. It also helps in identifying pancreatic inflammation or fluid collection. Ultrasound is often the first imaging study for suspected pancreatitis because it is safe, widely available, and does not include radiation risk.
CECT provides detailed imaging of the pancreas, helps in detecting necrosis, fluid collection, prochemist or other complications. It is particularly useful in severe cases to assess the limit and severity of the disease. Time is important, usually the symptom is done 48–72 hours after the onset to obtain optimal clinical information.
MRCP is a non-invasive imaging technique that imagines pancreatic and bile ducts. It detects stones, strictness, or ductal anomalies, causing acute pancreatitis. MRCP avoids radiation exposure and is useful for interfering or planning surgery, especially in patients where ultrasound or CT conclusions are indiscriminate.
The EUS combines endoscopy and ultrasound to provide high-resolution images of the pancreas. It is highly sensitive to detect small stones, ulcers, tumors or structural abnormalities. The EUS can guide therapeutic interventions such as stone removal or biopsy, making it a valuable tool in the management of matters of complex or recurrent acute pancreatitis.
