Chronic pancreatits
Introduction
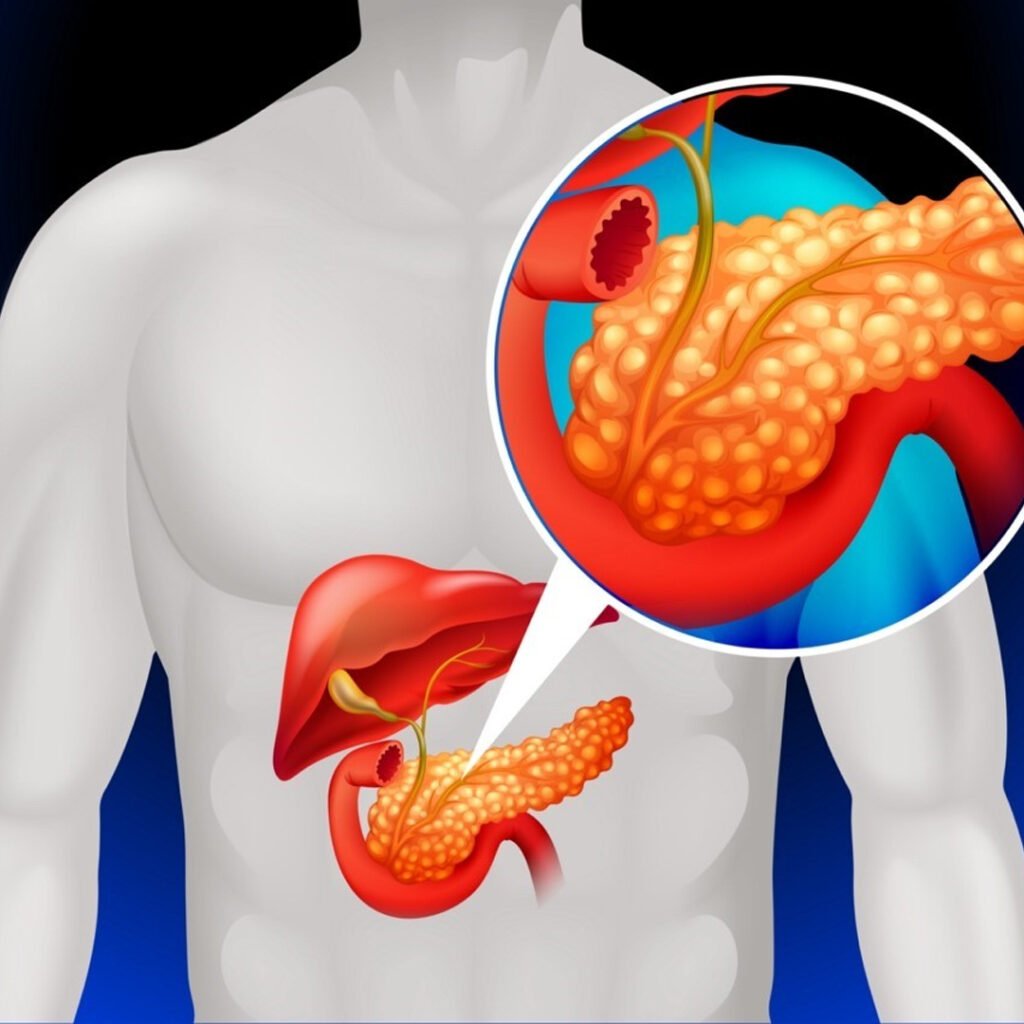
Chronic pancreatitis is a long -lasting inflammation of the pancreas that leads to permanent structural damage, resulting in impaired digestive enzyme production and hormonal imbalance. It usually develops gradually, causing progressive damage to recurrent abdominal pain and pancreatic function. Common causes include alcohol consumption, genetic factors, bile stones, smoking and autoimmune conditions. If left untreated, it can lead to diabetes, malabsorption and other serious complications.
Types of Chronic pancreatits
Alcohol
Excessive alcohol damages pancreatic tissue, causing frequent swelling and final functional loss.
Idiopathic chronic pancreatitis
It occurs without any identityable reason, often associated with genetic or unknown factors.
Hereditary chronic pancreatitis
Inherited genetic mutations cause the recurrent pancreatic inflammation, usually beginning in early life.
Autoimmune chronic pancreatitis
The immune system attacks pancreatic cells, which responds to fibrosis and corticosteroid therapy.
Causes of Chronic pancreatits :
- Excessive alcohol consumption causes frequent pancreatic inflammation and permanent tissue damage.
- Galstone blocks the pancreatic ducts, causing long -term inflammation and functional loss.
- Genetic mutations increase sensitivity to chronic pancreatic inflammation and fibrosis formation.
- Autoimmune disorders trigger immune attacks on pancreatic cells, damaging overall function.
- High triglyceride levels induce chronic pancreatic irritation and inflammation over time.
- Some drugs cause prolonged pancreatic damage, causing chronic pancreatitis development.
- The recurrent acute pancreatitis episode is ultimately the result of frequent pancreatic inflammation.
- Interest in pancreatic ducts by the tumor causes chronic inflammation and fibrosis.
- Smoking increases the risk of damage to chronic pancreatic tissue.
- Hypercasia leads to calcification in the pancreas, resulting in chronic inflammation.
Clinical features of Chronic pancreatits :
Persistent abdominal pain
Continuous upper abdominal pain reaches the back and worsens after meals.
Digestive problems
Poor digestion causes inflammation, gas and discomfort due to lack of enzymes.
Unexplained weight loss
The weight is reduced because the pancreas fails to absorb essential nutrients properly.
Fatty or oily stool
Fat in the stool causes smooth, dishonesty, and swimming due to digestion.
Diabetes
Damage to insulin-producing cells causes diabetes on the progression of the disease for a long time.
Symptoms associated with Chronic pancreatits:
- After eating, there is a continuous upper abdominal pain.
- Especially after heavy meals, repeated episodes of nausea and vomiting.
- Smooth, dishonest-cheer stool due to poor fat digestion and absorption.
- Unexplain due to improper digestion and absorption of nutrients.
- There is an increase in thirst and urination indicating the possible start of diabetes mellitus
- Frequent swelling and excessive gas formation after consuming fatty foods.
- Constant fatigue and weakness due to poor absorption of essential nutrients.
- Recruitment digestive discomfort leads to low hunger and food intake.
Investigations in Chronic pancreatits:
- Blood tests measure pancreatic enzymes such as amylase and lipase, liver function and blood sugar levels. Constant abnormal results indicate impaired pancreatic function and help diagnose associated complications such as diabetes or liver participation in chronic pancreatitis.
The ultrasound of the abdomen uses sound waves to detect pancreatic enlargement, calcification, fluid collection and ductal abnormalities. It is a non-invasive, first-rich imaging tool that usually evaluates structural changes in the pancreas seen in patients with chronic pancreatitis.
CT scans offer wide cross-sectional images of the pancreas, which reveal calcification, ductal delegation, pseudocysts and other abnormalities. It is highly effective in detecting structural damage caused by chronic pancreatitis and related complications.
The MRI with MRCP provides high-resolution images of pancreatic ducts and surrounding structures. It is particularly useful for evaluating ductal barriers, strictness, and early pancreatic tissue changes, providing better clinical accuracy than ultrasound or CT scans.
The EUS combines endoscopy and ultrasound to obtain highly wide images of the pancreas. It detects microscopic changes in pancreatic structure, small stones, fibrosis and ductal abnormalities, making it valuable for early diagnosis of chronic pancreatitis.
ERCP is an advanced clinical and therapeutic tool to imagine pancreatic and bile ducts. It detects barriers, strictness and stones and can also be used to interfere with stent placement or stone removal during the process.
This stool test measures the elastage level to assess the exocrine function of the pancreatic. The low fecal elastage indicates impaired enzyme secretion, which suggests malicious and poor digestion, usually associated with chronic pancreatitis and progressive pancreatic damage.
This test evaluates pancreatic function by measuring bicarbonate secretion after secretory administration. Less bicarbonate output indicates significant damage to the pancreas. It is useful to diagnose chronic pancreatitis of the early stage before having severe structural changes.
These tests assess enzyme secretions, bicarbonate levels and overall exocrine functions. They help detect malabsorption associated with chronic pancreatitis and nutrient deficiency, guiding dietary modifications and enzyme supplementation for better patient results.
Genetic testing identifies the mutation associated with hereditary chronic pancreatitis, such as PRSS1 and Spink1. It is particularly useful for a strong family history or patients with early onset, helps with initial diagnosis, consultation and preventive care plan.
