Gastro-oesophageal reflux
Introduction
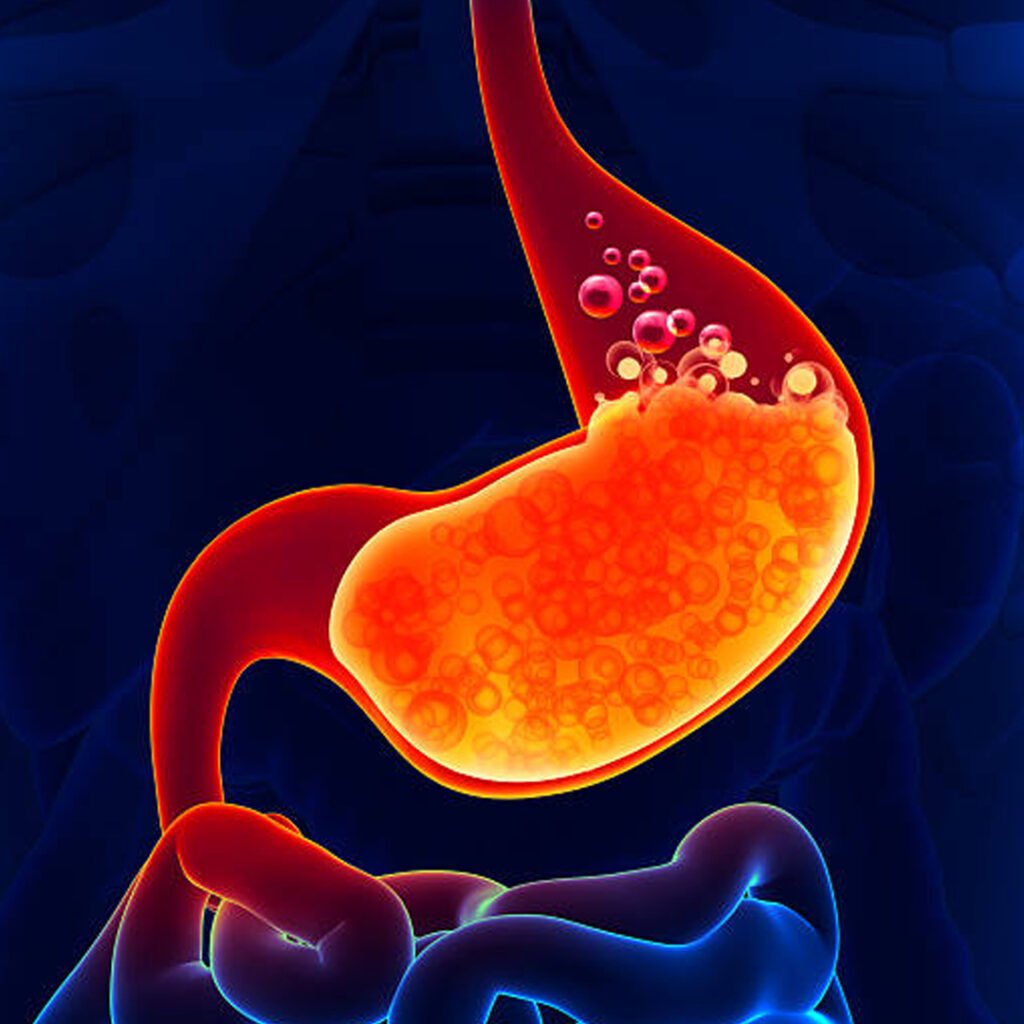
Gastro-ocefagel reflux disease (GERD) occurs when stomach acid or material flows backwards in the esophagus, harassing its lining. This reflux causes symptoms such as resentment, revival and chest discomfort. Over time, it can lead to complications such as osophagitis, strictness or barret esophagus. Contributing factors include obesity, certain foods, smoking, alcohol, and a weak lower osophageal sphinkter. GERD affects the quality of life and requires lifestyle modifications and medical management.
Types of Gastro-Ocephgal Reflux
Non-Erosive Reflux Disease (NERD)
Acid reflux causes specific symptoms without damage to the osophagal lining during endoscopy.
Irosive reflux disease (ERD)
Frequent acid reflux damages the osophagal lining, causing erosion or ulcers that appear during endoscopy.
Bhata with Barrett's Esophagus
Chronic acid exposure causes cellular changes to the esophagus, which increases the risk of cancer.
Additional-ocefagal reflux
Acid reflux affects the throat, lungs, or sinuses, causing symptoms such as coughs, ravages, or asthma.
Causes of Gastro-Ocephgal Reflux:
- Excessive consumption of spicy, fatty, or acidic foods can relax the lower osophageal sphinkter, which can cause acid reflux.
- Obesity increases abdominal pressure, pushing the stomach contents upwards in the esophagus, causing gastro-oasphagal reflux symptoms.
- Hiatal hernia occurs when the upper stomach pushes through the diaphragm, weakens the sphinkter function and causes reflux.
- Pregnancy increases abdominal pressure and hormonal changes, which relaxes the osophageal sphinkter and triggers acid reflux.
- Smoking weakens the lower osophageal sphinkter, reduces saliva production, and contributes to reflux, affecting acid neutralization.
- Consumption of alcohol disturbs the osophageal lining and relaxes the lower osophageal sphinkter to promote acid backflow.
- Excessive caffeine intake can relax the lower osophageal sphinkter, which increases the chances of acid reflux.
- Medications such as NSAID, Calcium Channel blockers and some sedatives can weaken the sphinkter, causing symptoms of reflux.
- The delayed stomach empties or increases gastrorious gastric pressure, promotes acid reflux in the esophagus.
- Tight fabrics around the abdomen increase intra-pat pressure, contributing to the gastro-ocefagel reflux episodes.
- Stress and anxiety can increase acid production and esophageal sensitivity, worsening reflux symptoms over time.
Clinical features of Gastro-Ocephgal Reflux:
Heartburn
A burning sensation occurs in the chest, often worsening after meals or when lying down.CKD is often found accidentally through regular blood tests. It is usually identified in high risk patients (eg, diabetes or high blood pressure).
Regurgitation
The content of acidic or sour abdominal stomach flows into the mouth, causing discomfort and poor taste.
Chest pain
Pains like sharp or pressure may occur, sometimes mimic the heart related conditions and require evaluation.
difficulty swallowing
Swelling, strictness, or esophagal narrowness causes pain and makes food or fluid difficult.
chronic cough
Acid reflux harasses the throat and airway, resulting in persistent cough, ravages, and throat discomfort.
Symptoms associated with Gastro-Oesophageal Reflux:
- A burning sensation in the chest or upper abdomen, often after eating or lying down.
- Sour or acidic abdominal content flows into the mouth, causing bad taste and discomfort.
- Chest pressure or sharp pain that can sometimes mimic heart problems.
- Inflammation or narrowness of the esophagus makes food or fluid painful or difficult.
- Acids that disturb the throat and airway causes frequent cough.
- Acid reflux can provoke vocal cords, causing ravages, throat irritation, or agony.
- Patients may feel persistent lumps or tightness in the throat due to reflux irritation.
- Frequent reflux can be the cause of nausea, sometimes causes vomiting or discomfort after meals.
Investigations in Gastro-Oesophageal Reflux:
- Endoscopy involves inserting a flexible tube with a camera to imagine inflammation, erosion, ulcers, or esophagus of barrett and insert a flexible tube in the abdomen. Biopsy can also be taken to assess cellular changes or to control maliciousness for accurate diagnosis.
This test measures the acid exposure in the esophagus in 24 hours using a thin probe. It identifies abnormal reflux episodes, correases symptoms with the incidence of acid, and endoscopy conclusions help to confirm the GERD diagnosis when it is normal or indiscriminate.
The esophagal manometry measures the pressure and dynamics of the esophagus and low esophagal sphincter. It helps evaluate the sphinkter function, detects dynamics disorders, and guides the decisions of treatment, especially before surgical intervention such as fundoplication for serious or refractory GERD cases.
The barium swallow involves the inclusion of contrast material to imagine the esophagus and abdomen under the X-ray. It delays structural abnormalities, hiatal hernia, strictness, or delayed vacancy, provides valuable information for diagnosis and planning treatment in patients with reflux symptoms.
During endoscopy, tissue samples can be collected from the esophagus. Biopsy helps in detecting inflammation, metaplasia, dysplasia or maliciousness. It is particularly useful in chronic GERD cases to assess the risk of barret’s esophagus or osophagal cancer and guide management.
The impedance pH monitors detect both acidic and non-acidic reflux in the esophagus. It provides detailed information about frequency, duration and type of reflux, which is particularly useful in patients with persistent symptoms despite acid-dominating therapy.
These studies assess the rate of emptying the stomach using radiolbelled food. Delayed gastric emptying can contribute to the reflux by increasing stomach pressure, providing insight into GERD pathophyliaology and by guiding proper medical or surgical management.
Blood tests can evaluate anemia, nutritional deficiencies or chronic inflammation markers. Despite not being clinical directly for GERD, they help assess complications such as long -standing reflux -related bleeding, malnutrition, or chronic disease.
These studies evaluate how esophagus leads food towards the stomach and how sphinkter works. Abnormal mobility can spoil the symptoms of reflux and direct therapeutic decisions, including dietary advice, medications or surgical intervention.
The secret blood test in the stool helps detect gastrointestinal bleeding caused by severe erosyvic reflux or ulcers. Positive findings indicate further investigation with endoscopy to detect bleeding sites and prevent complications such as anemia or chronic blood loss.
