Peptic ulcer disease
Introduction
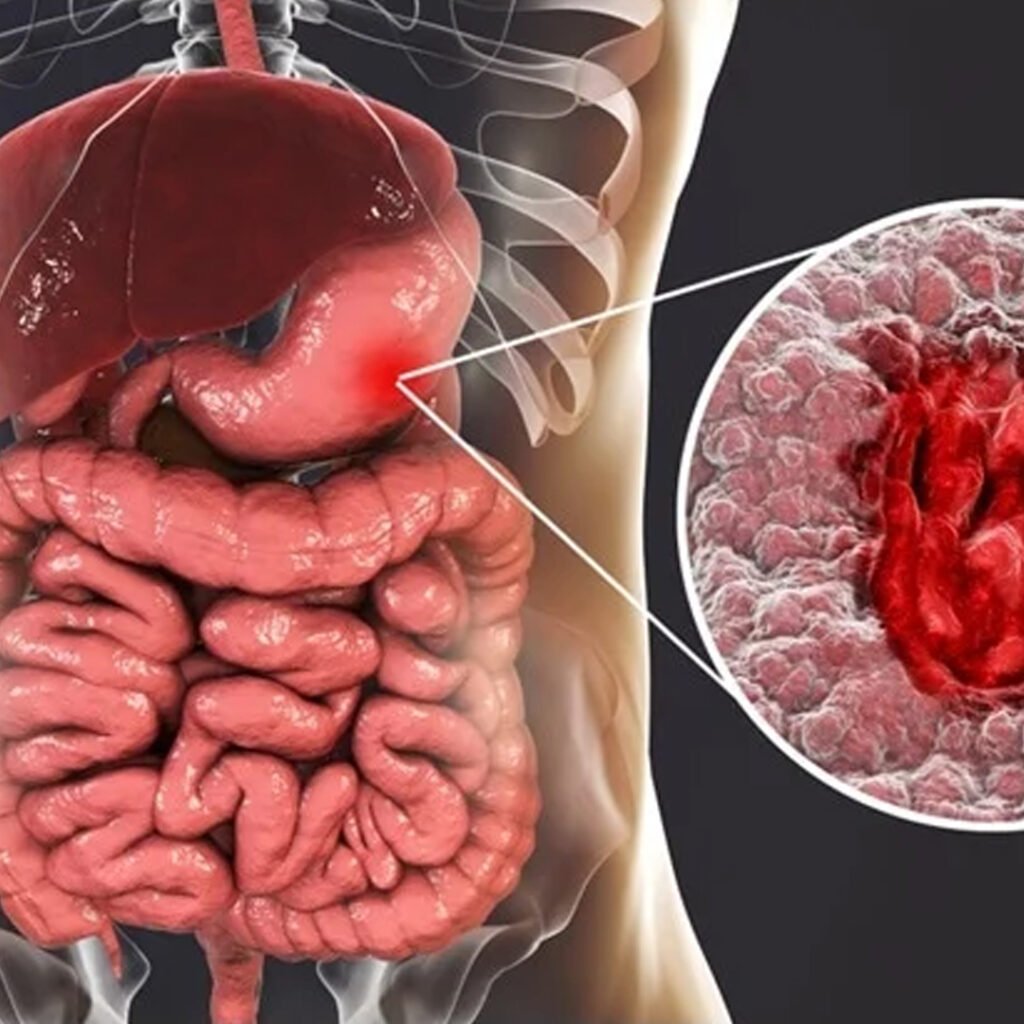
Peptic ulcer disease is a condition in which open lesions are called ulcers, on the internal lining of the abdomen, the upper intestine (duodenum), or on the lower esophagus. These ulcers develop due to imbalance between stomach acid and protective mechanisms, often due to factors such as helicobacter pylori infection, NSAID, smoking, alcohol, or excessive use of stress. Common symptoms include abdominal pain, swelling, resentment, nausea and indigestion.
Types of Peptic ulcer disease
Gastric Ulcer
Gastric ulcers are formed on the internal lining of the abdomen, mainly H. Due to pylori infection, NSAID use, or increase in acid production.
Duodenal Ulcer
Duodenal ulcers appear in the upper small intestine, commonly linked with H. pylori infection and excessive stomach acid secretion.
Esophageal Ulcer
Esophageal ulcers develop in the lower esophagus, often caused by chronic acid reflux, GERD, or frequent vomiting episodes.
Stress Ulcer
Stress ulcers occur during severe illness, trauma, burns, or surgery due to decreased blood flow and excessive stomach acid production.
Causes of Peptic ulcer disease
- Infection by Helicobacter Pylori bacteria damages the lining of the abdomen and increases acid secretion, which leads to the formation of ulcers.
- Excessive use of nonsteroidal anti-inflammatory drugs (NSAID) reduces stomach protection and causes lining irritation.
- The overproduction of stomach acid promotes the growth of ulcers in sensitive areas due to stress, lifestyle habits or medical conditions.
- Smoking weakens abdominal lining, delays ulcers treatment, and ulcers significantly increase the risk of recurrence.
- Excessive alcohol consumption irritates abdominal lining, increases acid secretions and damages protective mucosal obstacles.
- Chronic stress contributes to an increase in acid production and reducing the stomach protecting mechanisms, deteriorating the formation of ulcers.
- The family history of peptic ulcers increases personal sensitivity due to genetic and environmental factors.
- The zollinger-elison syndrome causes excessive gastric acid production from pancreatic or duodenal tumors, resulting in many ulcers.
- Continuous consumption of spicy, oily or acidic foods can worsen symptoms of ulcers and may delay natural healing processes.
- Some medical conditions such as liver cirrhosis, Crohn's disease, or chronic kidney disease increase the risk of ulcers.
Clinical features of Peptic ulcer disease:
Abdominal Pain
The upper abdomen causes irritation or pain pain, usually deteriorating on an empty stomach.
Indigestion
Patients experience swelling, discomfort and perfection after eating small amounts of food.
Nausea and Vomiting
Ulcers may cause nausea and sometimes vomiting, especially after heavy or acidic meals.
Heartburn
Frequent heartburn occurs due to acid reflux, causing burning sensations in the chest area.
Gastrointestinal Bleeding
Severe ulcers may lead to vomiting blood or passing black, tarry stools indicating bleeding.
Symptoms associated with Peptic ulcer disease:
- Constant upper abdominal pain that can improve after eating hunger or after deteriorating.
- Repeated swelling and perfection of the stomach, especially after consuming small food or snacks.
- Increased buried and excessive gas due to burning sensation of the stomach.
- Loss of appetite for noticeable weight loss in severe ulcer cases.
- Nausea occurring regularly, sometimes after meals or after an empty stomach.
- Burning of chest or throat due to acid reflux from the stomach.
- Fatigue and weakness due to loss of chronic blood from ulcers of bleeding.
- Dark, terry stool indicating possible internal bleeding from severe peptic ulcers.
Investigations in chronic kidney Peptic ulcer disease:
- Endoscopy helps imagine the abdomen, duodenum and esophagus, detecting ulcers, bleeding and inflammation. This tissue is to the biopsy h. The pylori infection allows to be confirmed or excluded maliciousness in suspected chronic peptic ulcer disease cases.
This non-invasive test detects active Helicobacter pylori infection by measuring exhaleed carbon dioxide after swallowing a urea solution. It is used to confirm the participation of bacteria in highly accurate and widely peptic ulcer disease diagnosis.
This test confirms the presence of infection, H in stool samples. Pylori identifies antigen. It is simple, non-invasive and useful for both early diagnosis and monitoring of the effectiveness of treatment in peptic ulcer disease.
A CBC chronic ulcer helps to detect anemia as a result of bleeding. Low hemoglobin levels or low hematocrit values indicate potential gastrointestinal blood loss, helping to evaluate possible complications such as ulcers’ severity and hidden bleeding.
These tests measure pancreatic enzyme levels to control pancreatitis, which can mimic the symptoms of ulcers. The level of elevated enzyme suggests pancreatic involvement or complications associated with severe peptic ulcer disease cases.
Patients have to swallow a barium solution, and X-ray imaging exposes the abdomen and duodenum. This test ulcers identify crater, gastric outlet barrier and other structural abnormalities when endoscopy is not easily available.
These tests measure the amount of acid produced by the stomach. Unusually high acid levels indicate hypersacresly states such as Zollinger-Elison syndrome, which increases ulcer risk and severity in older cases.
These tests evaluate liver and kidney health, ensuring safe use of ulcer medications. Impaired function can worsen symptoms or limit treatment options, especially in patients with chronic peptic ulcer disease complications.
Ultrasound detects complications like gastric outlet obstruction, perforation, or swelling around the stomach. It’s non-invasive and useful when ulcers cause associated fluid accumulation or surrounding tissue inflammation in chronic conditions.
A CT scan provides detailed imaging of the stomach and nearby structures, identifying perforations, obstructions, or suspected malignancies. It’s particularly valuable in complicated or non-healing chronic peptic ulcer disease cases.
