Chronic obstructive pulmonary Disease
Introduction
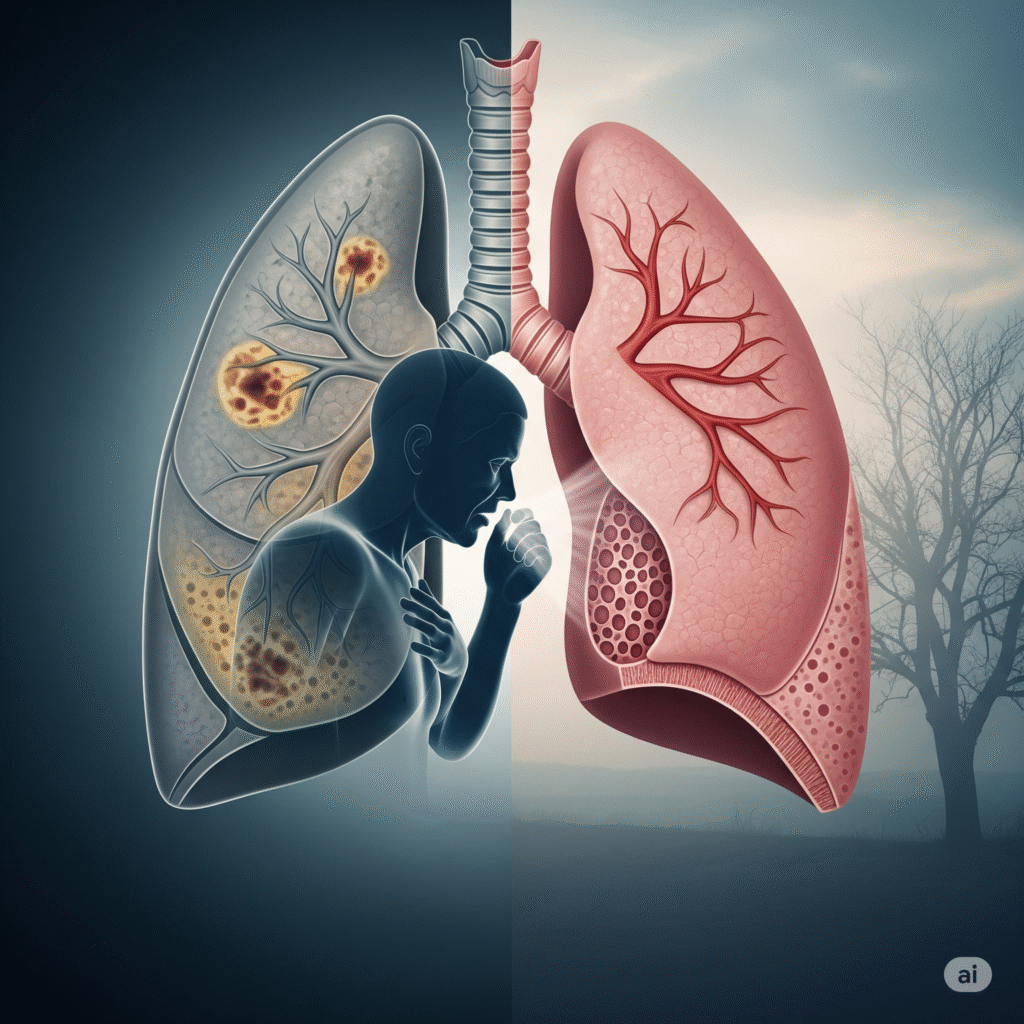
Chronic obstructive pulmonary disease (COPD) is a progressive lung condition that features frequent airflow boundaries and difficulties of breathing. This is usually caused by prolonged contact for cigarette smoke, dust, or irritability such as environmental pollutants. COPD contains a group of lung diseases that cause inflammation, structural damage and narrowness of airways, causing hard for air for air inside and out of the lungs.
Types of Chronic obstructive pulmonary Disease
Chronic bronchitis
Defined by chronic producers coughing at least three months in two consecutive years, due to inflammation of the airways and excessive mucus production.
Emphysema
The destruction of the alveolar walls is involved, causing loss of lung elasticity and reduces the surface area for gas exchange, resulting in breath withdrawal.
Asthma
A severe form of asthma that does not react well to standard drugs, causing a frequent airflow range similar to COPD.
Bronchiocytasis
Permanent spread of bronchi and damage, mucus accumulation and frequent respiratory infection due to frequent infection or inflammation.
Causes of Chronic obstructive pulmonary Disease
- risk. humanize text Smoking cigarette damages the airways and alveoli, causing chronic inflammation.
- Over time the secondhand smoke exposure causes the lung tissue equal to the same smoking.
- Air pollution from vehicles and industries disturb and denies the respiratory tract.
- Professional dust and chemicals cause long -term airways and lung damage.
- Biomas fuel increases the risk of COPD with indoor air pollution.
- Alfa -1 deficiency such as genetic factors make the lungs more weak.
- Childhood respiratory infections can limit the growth of the lungs and cause future problems.
- Chronic uncontrolled asthma can be irreversible airways narrow.
- Age reduces the function of the lungs, causing susceptible to damage to airways.
- The risk in the underdeveloped lungs increases as a result of low birth weight or premature birth.
Clinical features of Chronic obstructive pulmonary Disease:
chronic cough
Often the earliest symptoms, it may be drought or produce mucus, usually worse in the morning and continuously for years.
Spit production
Chronic inflammation in the airways and thick mucus often coughs due to overdom active mucus glands.
Breathing shortness
Gradually deteriorates over time, during the first hard work and after resting, due to the airflow range and reducing the elasticity of the lungs.
Wheezing
A whistle or scream sound during breathing due to compressed and inflamed airways.
Tiredness
Constant fatigue is because the body works hard to breathe and the tissues decrease oxygen delivery.
Symptoms associated with Chronic obstructive pulmonary Disease:
- Constant cough, often production of mucus, especially in the morning hours.
- Constant cough, often production of mucus, especially in the morning hours.
- Wheezing or whistling while breathing due to narrowing airway.
- Chest tightness or discomfort caused by airflow border and lung hyperfluence.
- Repeated respiratory infections such as bronchitis or pneumonia.
- Inconiting weight loss in advanced stages due to increased use of energy in breathing.
- Exercise tolerance less than fatigue and poor oxygen distribution to the body.
Cyneosis, a blue color of lips or fingers due to low oxygen levels.
Investigations in Chronic obstructive pulmonary Disease:
- Confirming the airflow range and the severity of the disease, assessing the volume and speed of air measures the function of the lungs.
Hyperinflated identifies the lungs, excluding other causes of symptoms such as pneumonia or heart disease.
Provides elaborate lung images to detect emphysema, airways change, or not visible on standard X-rays.
The gas exchange evaluates the level of oxygen and carbon dioxide in the blood to assess the severity of respiratory failure.
The non-invasive method to measure oxygen saturation is useful for ongoing monitoring of oxygen levels.
Bacteria analyzes mucus for infections or abnormal cells, especially during exercise.
Cronic detect heart stress or core pulmonary (right -sided heart problems) for lung disease.
Screen for genetic deficiency that increases sensitivity to early starting emphysema.
Assesses the patient’s ability to perform physical activity and determine oxygen requirements during diligence.
