Cirrhosis
Introduction
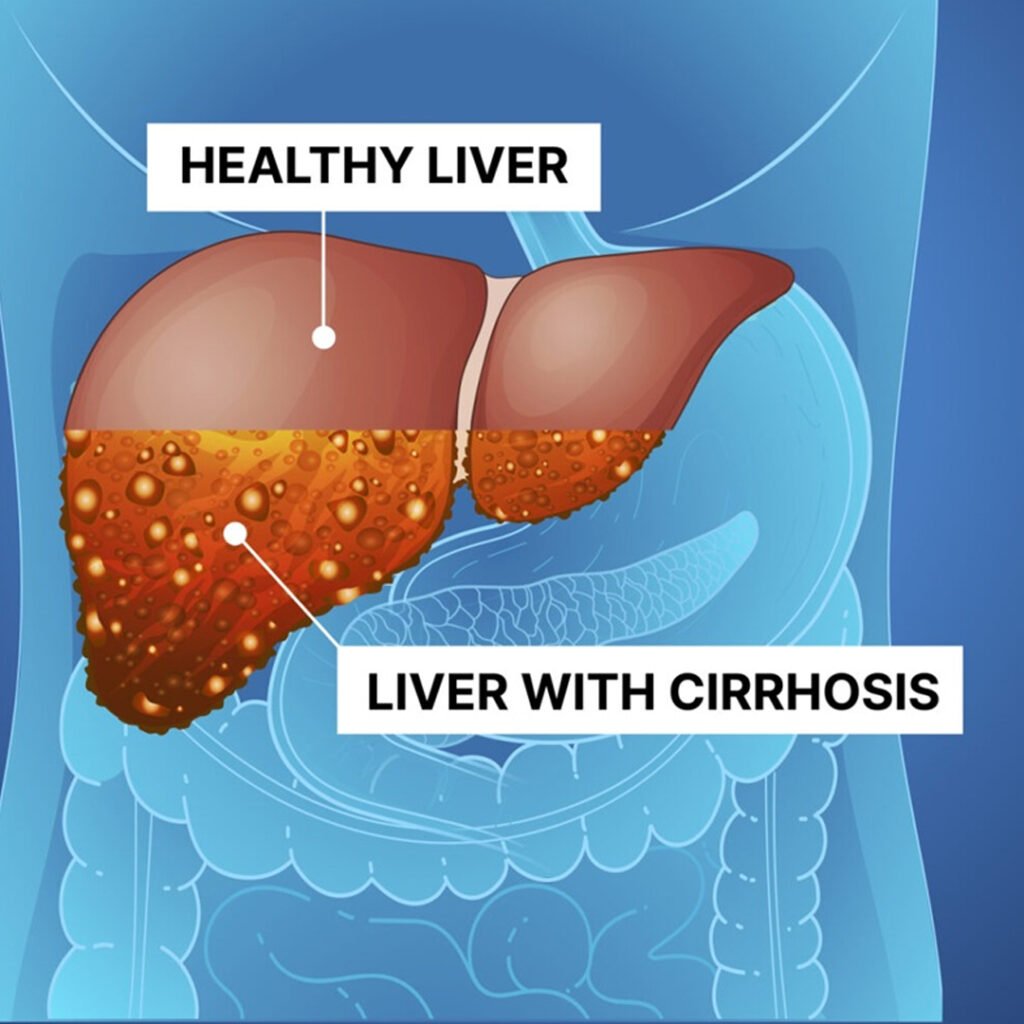
Cirrhosis is a chronic, progressive liver disease characterized by scarring and impaired liver function. It results from long-term damage caused by factors like alcohol, viral hepatitis, or autoimmune diseases. Over time, normal liver tissue is replaced by fibrous tissue, reducing liver efficiency and potentially leading to liver failure, complications, or portal hypertension.
Types of Cirrhosis
Alcoholic Cirrhosis
Caused by prolonged alcohol abuse, leading to liver scarring and impaired function.
Viral Cirrhosis
Develops due to chronic viral hepatitis B or C infection damaging liver tissue.
Biliary Cirrhosis
Results from long-term bile flow obstruction, causing bile accumulation and liver fibrosis.
Post-Necrotic Cirrhosis
Follows massive liver cell death due to toxins, drugs, or severe infections.
Causes of Cirrhosis
- Long-term heavy drinking damages liver cells, leading to inflammation, fibrosis, and cirrhosis.
- Persistent hepatitis B infection causes liver inflammation and gradual scarring over time.
- Long-term hepatitis C infection leads to progressive liver fibrosis and cirrhosis.
- Fat accumulation in liver cells triggers inflammation and scarring in non-alcoholic fatty liver disease.
- Immune system attacks liver tissue, causing chronic inflammation and fibrosis in autoimmune hepatitis.
- Blocked bile flow damages liver cells, resulting in bile accumulation and fibrosis.
- Autoimmune destruction of bile ducts causes chronic liver damage and cirrhosis in PBC.
- Progressive inflammation and scarring of bile ducts leads to liver fibrosis in PSC.
- Long-term use of hepatotoxic drugs can damage liver tissue and promote cirrhosis.
- Genetic disorders like hemochromatosis or Wilson’s disease cause metal accumulation, damaging the liver.
- Chronic infections or repeated liver injury can trigger fibrosis and eventual cirrhosis.
- Chronic heart failure or prolonged right-sided heart dysfunction causes liver congestion and fibrosis
Clinical features of Cirrhosis
Jaundice
Yellowing of skin and eyes occurs due to bilirubin accumulation from liver dysfunction.
Fatigue
Persistent tiredness develops because the damaged liver cannot efficiently metabolize nutrients and toxins.
Ascites
Fluid accumulates in the abdomen due to portal hypertension and reduced liver protein production.
Easy Bruising
Reduced clotting factor synthesis by the liver leads to frequent bruising and bleeding.
Hepatomegaly & Splenomegaly
Enlarged liver and spleen result from chronic inflammation and portal hypertension in cirrhosis.
Symptoms associated with Cirrhosis
- Reduced desire to eat occurs due to impaired liver function and digestive disturbances.
- Unexplained weight loss happens as the liver cannot properly metabolize nutrients.
- Nausea and vomiting result from liver dysfunction and toxin buildup in the body.
- Fluid accumulates in the abdomen due to portal hypertension and low protein levels.
- Persistent itching occurs from bile salt deposition under the skin.
- Decreased clotting factor production by the liver leads to easy bruising and bleeding.
- Toxin buildup in the bloodstream can cause confusion and mental changes.
- Bilirubin accumulation darkens urine, while impaired bile flow lightens stool color.
Investigations in Cirrhosis
- Measures liver enzymes (AST, ALT, ALP), bilirubin, and serum proteins to evaluate liver health. Abnormal results indicate liver cell injury, impaired bile flow, or reduced synthetic function due to cirrhosis.
Assesses red and white blood cells, hemoglobin, and platelets. Cirrhosis often causes anemia, leukopenia, or thrombocytopenia due to portal hypertension, hypersplenism, and bone marrow suppression.
Non-invasive imaging used to evaluate liver size, texture, nodules, and fatty changes. Detects early cirrhotic changes, ascites, and spleen enlargement for monitoring disease progression.
Provides detailed cross-sectional images of the liver, identifying fibrosis, regenerative nodules, hepatomegaly, and complications like portal vein thrombosis or ascites.
High-resolution imaging visualizes liver architecture, detects fibrosis, nodules, and vascular abnormalities. Helps assess disease severity and differentiate benign versus malignant lesions in cirrhosis.
Evaluates clotting ability, which is reduced in cirrhosis due to impaired synthesis of clotting factors. Prolonged PT indicates advanced liver dysfunction and bleeding risk.
Measures bilirubin levels to assess liver’s excretory function. Elevated bilirubin causes jaundice and indicates impaired bile processing or hepatocellular damage.
Monitors for hepatocellular carcinoma development, which is a common complication in patients with long-standing cirrhosis. High AFP levels suggest malignancy.
A sample of liver tissue is examined microscopically to confirm cirrhosis, assess fibrosis stage, and identify underlying etiology, such as alcohol, hepatitis, or autoimmune disease.
Detects esophageal and gastric varices caused by portal hypertension. Helps prevent life-threatening bleeding by guiding prophylactic treatment like banding or medication.
