Non-alcoholic fatty liver disease
Introduction
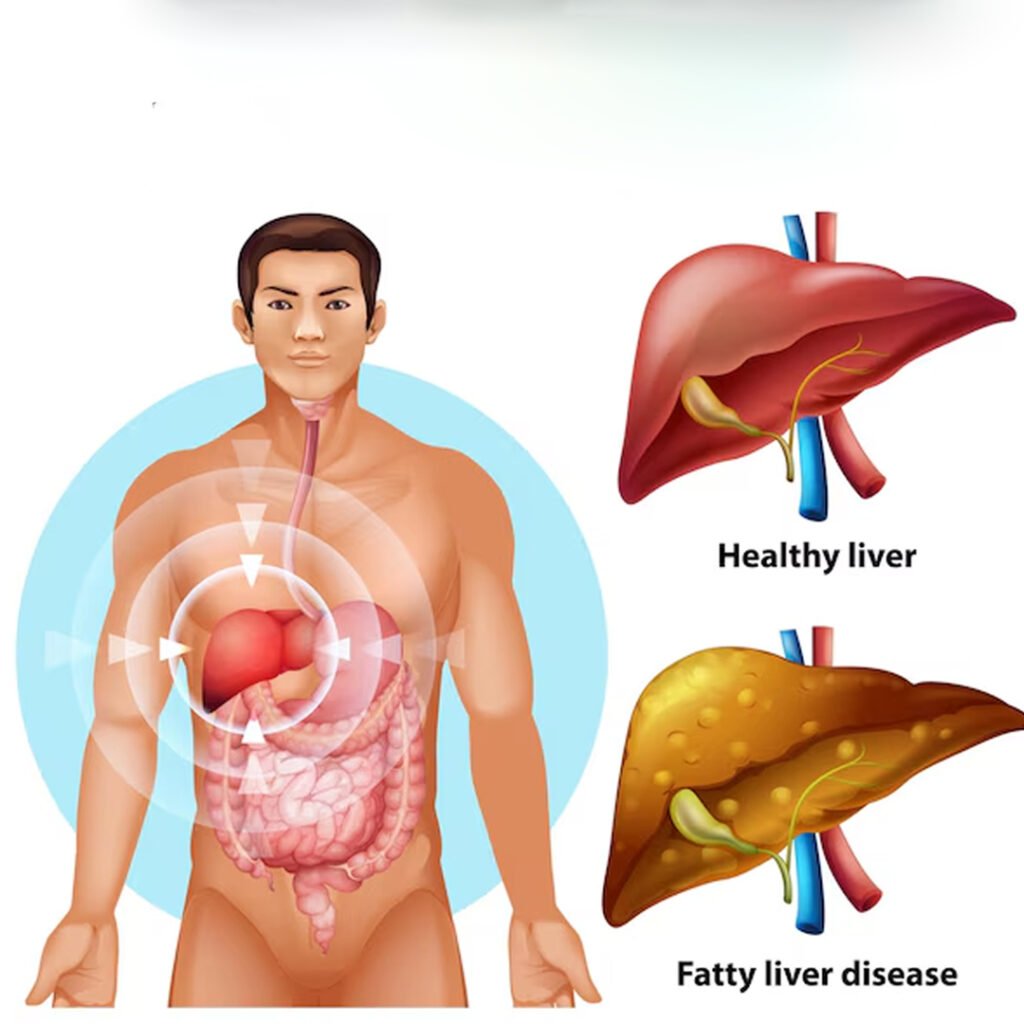
Non-alcohol fatty liver disease (NAFLD) is a common liver disorder characterized by excessive fat buildup in liver cells without significant alcohol consumption. It is closely associated with obesity, diabetes, high cholesterol and metabolic syndrome. If left untreated, NAFLD can progress to swelling, fibrosis, cirrhosis and even liver failure or cancer.
Types of Non-alcohol fatty liver disease
Simple Hepatic Steatosis
This is the initial stage where additional fat is formed in the liver, but there is no swelling or damage.
Non-alcohol steetohepatitis (NASH)
A more severe form where fat accumulation causes inflammation and liver cell damage, possibly progressed to fibrosis or cirrhosis.
Fibrosis
In this stage, the cause of frequent inflammation develops around the scar tissue liver cells, reduces its overall functionality and efficiency.
Cirrhosis
The most advanced phase, where the broad liver severely disrupts the function of the liver, is often leading to liver failure or risk of cancer.
Causes of Non-alcohol fatty liver disease
- Obesity increases fat accumulation in the liver, causing non-alcohol fatty liver disease.
- Insulin resistance causes improper fat metabolism, contributing to liver fat storage and damage.
- Type 2 diabetes increases the liver fat buildup due to impaired glucose and lipid metabolism.
- The level of high cholesterol and triglyceride promotes fat deposition within liver cells, deteriorating the condition.
- Liver fat accumulation is caused by processed foods and a poor diet rich in sugars.
- The sedentary lifestyle reduces fat burning, gradually promotes fat buildup in liver tissues.
- Metabolic syndrome combines obesity, hypertension and diabetes, which increases fatty liver disease risk.
- Rapid weight loss or extreme dieting can trigger fat release, affecting liver health.
- Polycystic ovary syndrome (PCOS) affects the hormone, increases the chances of developing fatty liver disease.
- Genetic factors make some individuals more prone to develop fatty liver problems quickly.
- Some drugs, such as corticosteroids, liver fat accumulation and loss, increase liver function.
- Sleep apnea causes oxygen deficiency, promotes liver inflammation and worsens fatty liver disease.
Clinical features of NAFLD:
Stomach discomfort
Patients may experience mild pain or discomfort in the upper right stomach due to liver enlargement.
Persistent fatigue
Constant fatigue and low energy levels are because fat accumulation affects liver function and metabolism.
Unexplained weight loss
Some patients unpredictually lose weight because the liver struggles to process nutrients and energy efficiently.
Enlarged Liver (Hepatomegaly)
Liver enlargement is common and can be detected during physical examination or imaging clinical processes.
Liver enzymes elevated
Blood tests reveal the level of often raised liver enzymes, indicating liver inflammation and potential damage progression.
Symptoms associated with Non-alcohol fatty liver disease
- Constant fatigue and low energy levels occur as liver function gradually declines due to fat accumulation.
- Mild pain or discomfort in the upper right abdomen result results from liver growth and inflammation.
- Unexplain loss can occur when the liver struggles to properly process fat and nutrients.
- Loss of appetite after small meals and quick feeling indicate impaired liver function and digestion.
- Stomach swelling or leg edema decreases, which is caused by fluid retention due to low liver efficiency.
- Advanced liver damage appears in severe stages of skin and eyes (jaundice).
- Difficulty and persistent confusion in focusing when the liver dysfunction greatly affects the function of the brain.
- Nausea and topical vomiting occurs because fat buildup affects liver health and digestive processes.
Investigations in Non-alcohol fatty liver disease
- LFTs measure enzyme levels like ALT and AST in the blood. Elevated enzyme levels indicate liver inflammation or damage. It helps assess the liver’s overall functionality and detect the extent of fat-induced injury, making it one of the first diagnostic steps for NAFLD.
-
An abdominal ultrasound is a commonly used, non-invasive imaging test to detect fat deposits in the liver. It provides clear visuals of liver texture and identifies fatty infiltration early. It’s widely preferred as an initial screening tool for NAFLD due to its safety and effectiveness.
-
FibroScan measures liver stiffness and elasticity using ultrasound waves. It helps evaluate the extent of fibrosis and scarring caused by fatty liver disease. This quick and painless method is often used to differentiate between simple steatosis, NASH, and cirrhosis in NAFLD patients effectively.
-
A CT scan creates cross-sectional liver images to measure fat accumulation and detect structural changes. Though less sensitive than MRI, it is useful in ruling out other abdominal issues. Doctors typically recommend it when ultrasound findings are inconclusive or additional complications are suspected.
-
Liver biopsy is the gold standard for diagnosing and staging NAFLD. A small tissue sample is extracted and examined under a microscope to identify fat accumulation, inflammation, and fibrosis. Though invasive, it provides the most accurate information about disease severity and future treatment planning.
-
These tests help check blood sugar levels and long-term glucose control. Since NAFLD is often linked with diabetes and insulin resistance, monitoring glucose levels is essential. Abnormal results indicate metabolic syndrome, which worsens fatty liver progression and requires proper management alongside liver treatment.
-
The lipid profile measures cholesterol, LDL, HDL, and triglyceride levels. High levels of bad cholesterol and triglycerides are strongly associated with NAFLD. This test helps doctors identify metabolic risk factors contributing to fatty liver disease and guides dietary, lifestyle, and medical treatment strategies.
-
Serum ferritin tests measure stored iron levels in the body. Elevated ferritin levels indicate liver inflammation and oxidative stress, which can worsen NAFLD. Doctors use this test to assess liver health and exclude other iron-related disorders, such as hemochromatosis, which may complicate the disease.
-
AFP testing is used to monitor potential liver cancer development in advanced NAFLD cases. Higher AFP levels may indicate liver cell damage or hepatocellular carcinoma. This test is particularly important for patients showing signs of cirrhosis or extensive fibrosis, helping detect cancer early for timely intervention.
-
CBC measures red blood cells, white blood cells, and platelets to evaluate liver-related complications. Abnormal counts may indicate inflammation, infection, or bleeding tendencies due to advanced liver dysfunction. This test, when combined with LFTs, provides a clearer picture of overall liver health.
-
Genetic testing helps identify mutations or hereditary factors that increase susceptibility to NAFLD. It is especially useful in patients with a strong family history of fatty liver disease or metabolic disorders. Early detection through genetic analysis enables personalized treatment plans and better preventive care strategies.
